The Challenges With Implanted Medical Devices
Electronics have revolutionized the medical field, enabling constant monitoring, automated drug delivery, and secure remote data access for healthcare professionals. But, the transition from external or wearable systems to fully implanted devices introduces a complex set of engineering challenges that go far beyond standard product development.
Perhaps the most fundamental of these is biocompatibility, as every material used in an implant must remain inert within the body for years, resisting immune reactions, chemical degradation, or toxic leaching, all while maintaining its mechanical and electrical performance under conditions that are far from laboratory-clean. This alone eliminates many high-performance materials that are commonplace in consumer electronics, forcing engineers to design within a narrow, medically approved palette.
Power delivery is another formidable obstacle, since once a device is implanted it cannot be conveniently accessed for maintenance or battery replacement. Any integrated power source must therefore be exceptionally long-lasting, capable of harvesting energy from the body or the environment, or suitable for wireless recharging. Unfortunately, traditional battery chemistries often contain toxic substances that could be fatal if leakage occurs, and surgical intervention to replace a failing battery carries significant risks.
Wireless charging might appear to solve this problem, but it brings its own set of difficulties. The depth of the implant within the body can severely limit energy transfer efficiency, as human tissue absorbs radio frequency energy and reduces coupling effectiveness. Even when charging is technically possible, the amount of power lost during transmission may render the approach impractical, especially for devices that must power multiple subsystems such as sensors, microcontrollers, and wireless communications modules simultaneously.
For these reasons, developing implanted medical electronics demands innovation across multiple disciplines, requiring not just advances in circuit design but also in material science, biomedical engineering, and long-term reliability testing, fields that must come together to produce devices that are safe, functional, and capable of operating unseen beneath the skin for years without failure.
Korean Researchers Achieve Breakthrough in Ultrasound Wireless Charging for Medical Implants
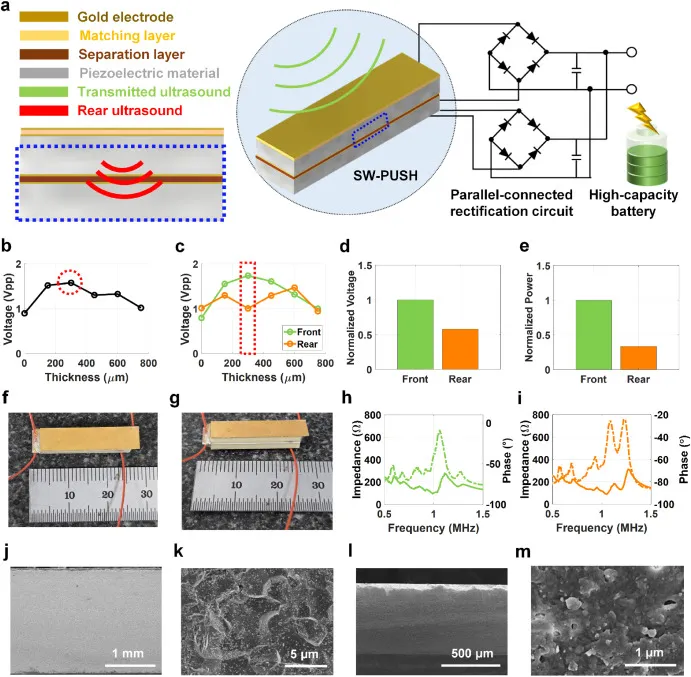
Recently, a research team at the Daegu Gyeongbuk Institute of Science and Technology (DGIST) in Korea have developed a highly efficient wireless charging system for implantable medical sensors, using ultrasound rather than traditional radio frequency methods. Their approach, centered around a “sandwich-structured” piezoelectric energy harvester (SW-PUSH), has demonstrated the ability to fully charge a commercial battery in under two hours, an achievement that could significantly extend the practical capabilities of implanted electronics.
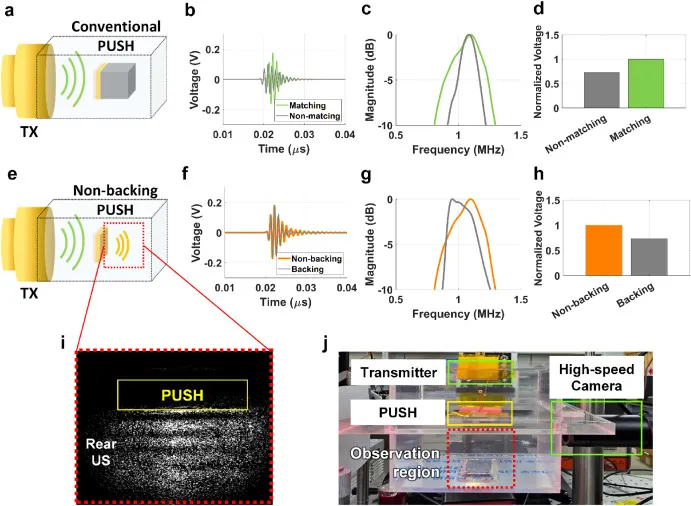
The harvester itself is composed of two stacked piezoelectric layers. The front layer captures incoming ultrasound energy and converts it into electricity, while the rear layer recovers residual ultrasound that would otherwise be wasted, adding to the total power output. By combining the contribution from both layers, the device achieves a remarkable power density of 497.47 mW/cm² and a total power output of 732.27 mW in water, over 20% more efficient than conventional designs in similar conditions.
To maximize performance, the DGIST team precisely matched the harvester’s dimensions to the ultrasound transmitter’s beam characteristics. The transmitter generates a main lobe width of 6.4 mm × 28 mm at a focal length of 30 mm, leading to a SW-PUSH footprint of 6.4 mm × 23 mm × 4.6 mm. Each unit is built from two PZT-5H piezoelectric components separated by a 300 μm epoxy-glass matching layer, with both surfaces coated in Cr/Au to optimize energy transfer. The PZT-5H thickness of 2.0 mm was chosen to achieve a 1 MHz operating frequency, identical to the transmitter.
In testing, the system charged a 140 mAh battery in just one hour and 40 minutes at a submerged distance of 30 mm. When tested through 30 mm of biological tissue, a 60 mAh battery reached full charge in one hour and 20 minutes, delivering at least twice the power output of previous ultrasonic charging systems.
“This research effectively harvests ultrasound energy, which has not been fully utilized in the past, for wireless charging of implantable medical devices. We aim to commercialize a system capable of fully charging within one hour by combining this ultrasound-based wireless charging technology with high-efficiency semiconductor components,”
- Professor Jinho Chang\, DGIST’s Department of Electrical Engineering and Computer Science.
Is this design viable for implanted medical devices?
While many scientific announcements in the field of implanted medical devices often amount to incremental progress, interesting in concept but with little immediate practical impact, this development from the DGIST team is refreshingly different. Their ultrasound-based wireless charging system is not merely a laboratory curiosity but a plausible, scalable solution for powering implantable electronics. The reported energy capacity of 140 mAh, while it might sound limited compared to everyday gadgets, is actually quite substantial for implanted systems. It comfortably supports essential components such as microcontrollers, sensors, and even certain actuators or motors that require more power. This kind of capacity opens the door for more sophisticated, autonomous implanted devices that can do more without the constant worry of battery depletion.
Equally important is the charging time, around one hour and forty minutes under realistic conditions, which fits well within practical use scenarios. For example, imagine a patient simply clipping on a magnetic charging fixture that aligns perfectly with the implant beneath the skin. This is far more convenient and less invasive than repeated surgeries for battery replacement, something that currently limits the longevity and feasibility of many implantable devices.
The use of ultrasound rather than traditional RF or magnetic induction also offers a pathway to deeper implants where electromagnetic coupling falters, solving a major technical bottleneck.
Overall, this technology has the potential to transform the landscape of implantable medical devices, making long-term, reliable operation far more achievable than before. It’s rare to see research that so clearly bridges the gap from experimental prototype to real-world application, and this wireless charging device is undoubtedly one of those breakthroughs.
While there are still hurdles to clear before mass commercialization, this is precisely the kind of innovation that can push medical electronics out of the lab and into everyday healthcare, improving patient outcomes and quality of life.